Diabetes mellitus and the eyes
In diabetes blood glucose levels are an important – but by no means the only factor influencing the cause and consequences of diabetes mellitus.
-
CAUSES
Diabetes is related to sugar metabolism. However, elevated blood glucose levels are not the sole cause of diabetes, as was long believed. This is because even perfect blood glucose control cannot prevent the progression of diabetes. In therapy, the adjustment of blood glucose and blood pressure and, especially in type 2 (adult-onset diabetes), body weight and exercise play an essential role. These factors are treatable, and influence the progression of the disease. Hereditary factors and lifestyle habits such as diet, nicotine and alcohol consumption and fat metabolism are much more difficult to influence. The cause of the disease is probably either a regulatory disorder of the immune system with damage to the pancreas (type 1, juvenile diabetes) or a reduced sensitivity of the body’s cells to insulin (type 2). Diabetes mellitus affects the entire body.
-
GENERAL, EXPLANATION OF TERMS
The eyes are also affected by diabetes. After age-related macular degeneration, the involvement of the retina in the eye in diabetes (diabetic retinopathy) is the second most common cause of visual impairment in Europe and North America. In the age group of 20 to 70 years, diabetes is the most common cause of blindness. In Germany, diabetes, the most common metabolic disease, affects approximately 8-10 million people (Deutsche Diabetes Gesellschaft 2021). For Switzerland, the incidence is estimated to be around 500,000 people. The incidence of diabetes increases up to 16% in men and 12% in women between 75 and 84 years. In recent years, diabetes has increased significantly, especially in men, in parallel with the number of overweight people. In the meantime, type 2 diabetes has developed into a worldwide epidemic and today causes direct and indirect costs of 1.5 to 4 billion Swiss francs in Switzerland (FOPH estimate 2014).
When diabetes is discovered, almost 18% of type 2 diabetics already have changes in their eyes. Good vision is often mistakenly equated with a healthy retina that does not require treatment. However, visual disturbances are a late symptom that only appear after a long period of illness. The most common cause of visual disturbances in diabetes is swelling of the center of the retina (macular edema), which occurs more frequently in type 2 diabetes and affects both eyes in 45% of cases. The relationship of individual factors to the progression of the disease is becoming better understood. As a result, treatment is improving. Due to better treatment of damage to larger vessels, cardiovascular sequelae and their complications have been significantly reduced in the last 10-15 years. Due to the aging of the population, the number of diabetics will continue to increase. More and more diabetics reach later stages of diabetes, where damage to small vessels (microangiopathy) is in the foreground. This is most evident in the kidneys (nephropathy), nerves (neuropathy) and retina (retinopathy).
-
DIAGNOSTICS
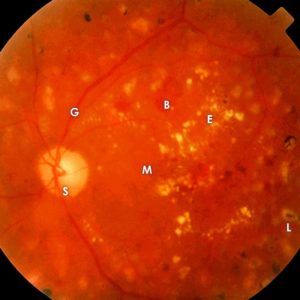 Advanced diabetic retinal damage B = hemorrhage, E = protein deposition, L = laser focus, S = optic nerve, G = vessels, M = macula: site of sharpest vision.
Advanced diabetic retinal damage B = hemorrhage, E = protein deposition, L = laser focus, S = optic nerve, G = vessels, M = macula: site of sharpest vision.Elevated blood glucose levels and blood pressure lead to damage of the small vessels and to oxygen deficiency in the eye. The two main problems resulting from this are diabetic macular edema and diabetic retinopathy. In diabetic macular edema, the damage to vessels and tissues causes fluid to leak into the center of the retina (the macula). This swelling directly worsens vision. For diagnosis, a cross-sectional image of the retina can be taken (optical coherence tomography). OCT also allows to determine the success of the therapy.
Diabetic retinopathy is caused by damage to the vessels outside the retina. In the examination, the ophthalmologist sees hemorrhages, swellings, small infarcts, and vascular changes. Color imaging of the retinal vessels (fluorescein angiography) is necessary to see details. In advanced stages, new blood vessels may grow uncontrollably.
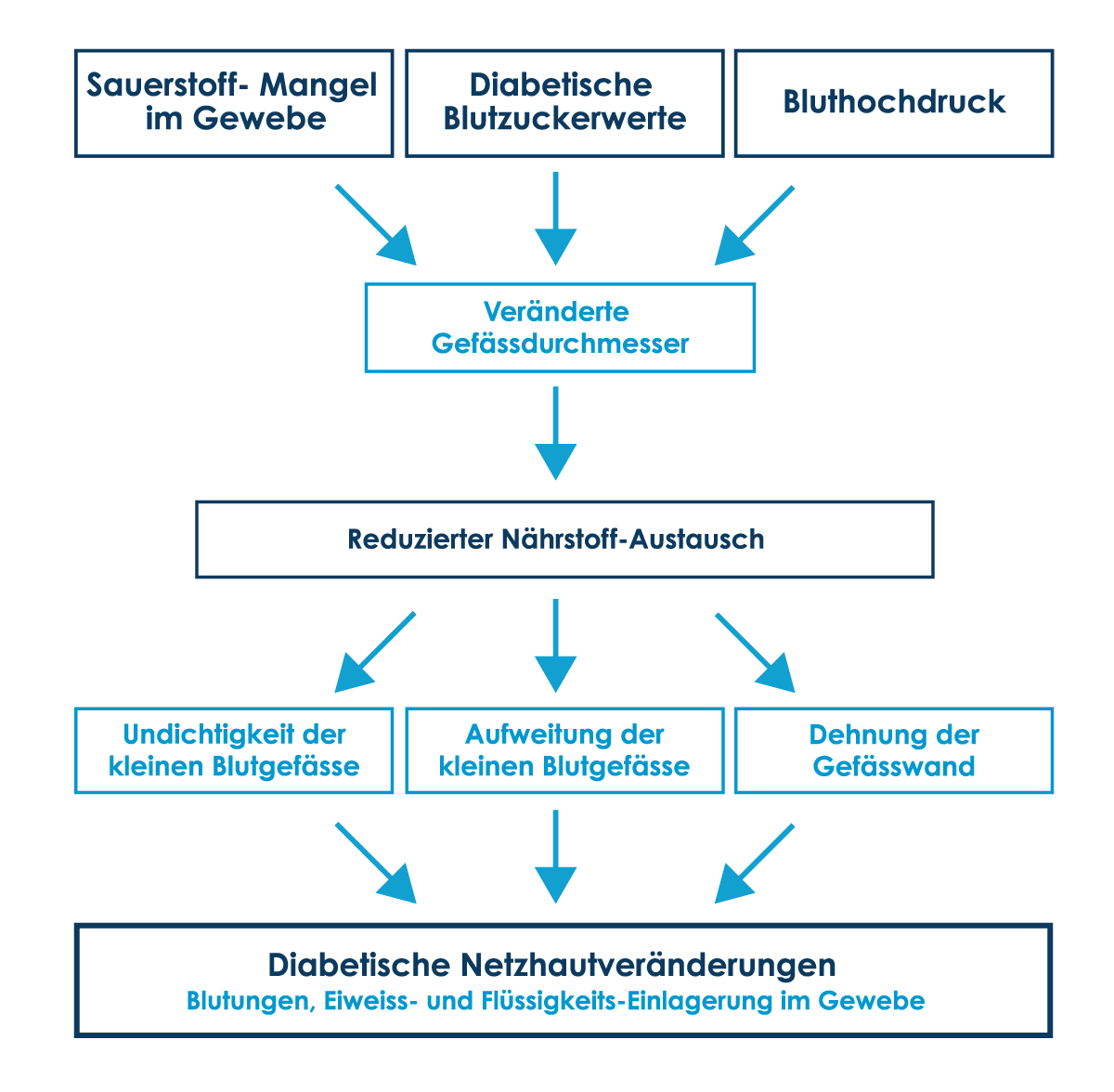
Causes and consequences of the diabetic metabolic disease
-
THERAPY
Since the 1980s, laser therapy has been core element in the treatment of diabetic retinal changes. Non-perfused areas of the retina are treated with laser. As a result, the areas with a better blood supply receive more oxygen. Laser therapy does not improve vision, but it significantly reduces the risk of severe vision loss in the long term.
A visual disorder caused by diabetes used to be treatable only if it was a hemorrhage into the interior of the eye (the vitreous body). Once damage to the center of the retina was discovered as the cause, nothing more could be done except improving blood sugar and blood pressure control, which is largely why more than 20% of late-stage diabetics went blind. Since about 2010, there are new drugs that directly stabilize the vessels in the eye. These are injected with a fine syringe into the vitreous cavity in the eye. This very expensive treatment leads to a rapid recovery of visual acuity, and preliminary stabilization of the retina. It is effective only for a short time (1-3 months) but can be repeated if necessary. When long-term stability of vision is achieved with laser and better diabetes control, often only a few injections are needed. However, it often takes more than a year to achieve this. These and newer drug treatments that directly target the supporting, and nourishing cells of the blood vessels are currently being clinically tested. Surgical procedures, especially vitrectomy (removal of the vitreous body), are thus less often necessary, and often only when drug options have been exhausted.
-
SUMMARY
The most important thing for long-term preservation of visual function, and quality of life is consistent blood glucose and blood pressure control. High and fluctuating blood glucose levels cause long-term damage to the small retinal vessels. High blood pressure accelerates the progression of diabetic eye changes and their transition into an aggressive form.
To avoid severe damage caused by diabetes, the eyes of all patients with diabetes mellitus must be checked regularly, at least once a year, by their personal ophthalmologist and treated in time before pronounced visual disturbances occur.
At the Berne Eye Clinic we offer the most complex control and therapy methods, and care for patients with diabetes mellitus together with the personal ophthalmologists close to the patient’s home.

