Retinal detachment
Retinal detachment (medical term: Amotio/Ablatio retinae) is a clinical picture in which the inner part of the retina with the visual cells detaches from the underlying layer (retinal pigment epithelium).
The retinal pigment epithelium supplies a large part of the retina with oxygen and nutrients and removes metabolic waste products.
In the case of a retinal detachment, the supply of the retina is no longer sufficiently ensured, so that if left untreated can lead to blindness of the eye, since the retina (especially the photoreceptors) atrophies. Therefore, a retinal detachment is a relative emergency that requires rapid ophthalmologic treatment (usually surgery).
-
CLASSIFICATION, RISK FACTORS
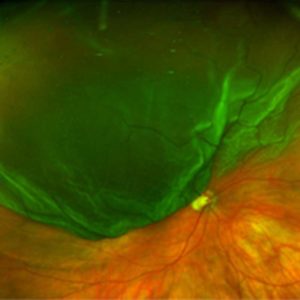 Retinal detachment in the upper part of the retina
Retinal detachment in the upper part of the retinaThe frequency of a retinal detachment is about 1 person per 10,000 persons per year. Retinal detachment occurs more frequently between the ages of 60 and 70, which coincides with a (naturally then often occurring) posterior vitreous detachment, but also with cataract surgery.
CLASSIFICATION:
Ruptured Retinal Detachment (Rhegmatogenous Amotio retinae):
This is the most common subtype of retinal detachment. A tight attachment or pulling of the vitreous body can cause tears or holes in the retina, through which fluid can get under the retina. Retinal detachment usually begins in the outer areas of the retina and can progress within hours or days to the visual center.
Risk factors for retinal detachment due to tearing:- Nearsightedness: Near-sighted eyes are usually longer than normal-sighted eyes and show more weak points, cracks and holes.
- Previous eye operations (e.g. cataract surgery)
- Congenital or acquired weaknesses of the retina
- Systemic connective tissue diseases (e.g. Marfan syndrome, Ehlers-Danlos syndrome)
- Eye injuries
- Retinal detachment in the other eye
- Familial high incidence of retinal detachment
Retinal detachment due to traction (Tractive Amotio retinae):In some diseases (e.g. diabetes, vascular occlusion, inflammation) connective tissue membranes can form on the retinal surface or under the retina. When these membranes contract, tension on the retina occurs and the retina detaches from the retinal pigment epithelium.
Aqueous retinal detachment (Serous Amotio retinae):
In this subtype, fluid accumulates between the retina and the pigment epithelium without mechanical cause. Causes can be inflammations or tumors.
-
SYMPTOMS
A retinal detachment is painless and becomes noticeable by a progressive restriction of the visual field.
Typical early symptoms of retinal detachment due to tearing can be:- Perception of lightning
- Perception of black spots (“Mouches volantes”, sooty rain)
- Perception of a shadow; at the beginning mostly in the outer field of vision, increasing towards the center; only when the shadow reaches the center, there is a loss of visual acuity as a late symptom
- visual impairment
-
DIAGNOSTICS
The suspicion of a retinal detachment requires a quick ophthalmological examination (within 1 day, in exceptional cases maximum 2 days).
To diagnose a retinal detachment, the ophthalmologist uses various examination methods. These include taking the patient’s medical history, checking risk factors, dilation of the pupil and capturing and analyzing the retinal reflection. Further examination methods such as ultrasound, optical coherence tomography (OCT) or retinal cameras support the ophthalmologist in making a diagnosis or documenting the course of the disease. -
TREATMENT
Depending on the extent and location of the retinal detachment, a different procedure may be considered.
For smaller retinal tears or retinal holes, a laser treatment (laser retinopexy) or a cold treatment (cryocoagulation) can be applied. The treatment artificially induces scarring, which is the prerequisite for the retina to grow firmly to the eye wall. This only works (as with spot welding) as long as the retina is still in contact with the layer below.To treat a retinal detachment, the forces that caused the retina to tear must be relieved. This can be achieved by a depression of the eye wall through external pressure, for example by means of a plastic seal or a plastic band around the eye (cerclage).
If this procedure is not enough to stabilize the retina, a so-called vitrectomy is necessary. Here, under local or general anesthesia, the vitreous body behind the lens of the eye is removed and the eye is filled with air, gas or silicone oil at the end of the procedure, depending on the stability of the retina.
In the case of a serous (aqueous) retinal detachment, treatment of the underlying disease (inflammation, tumor) should normally lead to reattachment of the retina.
-
PROPHYLAXIS, PROGNOSIS
The prognosis of a retinal detachment depends, among other things, on the location, extent and the time between the appearance of the first symptoms and treatment. In the case of small retinal detachments located far away from the center of the retina, which can be quickly treated surgically, a good recovery or preservation of visual acuity is usually possible. If the center of the retina is also detached and/or treatment is delayed for several days, the original visual function is usually no longer achieved. If a retinal detachment remains untreated, there is a risk of slow painful shrinking of the eye (phthisis bulbi).
Regular (at least annual) routine ophthalmological check-ups are essential, especially for patients with risk factors for retinal detachment (e.g. myopia, retinal detachment in the other eye, eye injuries). In the case of typical symptoms of retinal detachment (see above, including perception of lightning, “Mouches volantes”, shadows), a quick ophthalmological presentation (within 1 to 2 days at the latest) should be made, since in the presence of retinal tears or holes, immediate treatment with a laser can prevent retinal detachment in some cases.
-
AFTER YOUR OPERATION
Contact us if you experience pain or sudden redness. The same applies if your vision suddenly deteriorates or if you notice shadows or flashes.
A scratchy feeling, tearing or a sensation of a foreign body in the operated eye is normal in the first two days. Double vision and increased glare is also possible. You may also experience double vision and see increased glares.
During daytime a bandage is not necessary. You can protect the eye as you wish with glasses or sunglasses.
The operated eye is treated for a few weeks with TobraDex eye drops:
TobraDex Dosage (unless otherwise prescribed)
Shake well before use, one drop in each operated eye at the approximately the following times:8 am12 am4 pm8 pm
Your ophthalmologist will inform you when you can reduce dosage and when you can drive again at your follow-up examination.Permitted are:
- Showering and hair washing, keeping the operated eye closed. No soap or shampoo should enter the operated eye.
- Light work, general activities of daily life, bending, light gymnastics, lifting of loads up to 10kg.
- Walking, in sunny weather you can protect your eyes with sunglasses.
- Television, reading and writing as long as you feel comfortable.
Prohibited:- Rubbing or pressing your eyes or squinting hard.
- Lifting of loads over 10kg in the first week.
- Working in the garden or stable during the first two weeks.
- Weight training and swimming during the first two weeks.
- Driving, until the permission is given by your treating ophthalmologist.
- Stay at an altitude above 800 m.a.s.l. for a week.
Follow-up examinations take place as agreed.Usually appointments are made 1-2 days after the operation and after one month, after one week by your private ophthalmologist.
Newly prescribed glasses usually only makes sense after 4-6 weeks after the operation. Temporary glasses can be used during this time.
In case of emergency (also on Saturday, Sunday and on holidays) you can reach an ophthalmologist at our eye clinic at the following number:
031 311 12 22

