Diseases of the Macula
Diseases of the macula are diseases that affect the center of the retina, and thus also the area of sharpest vision.
-
INTRODUCTION
Diseases of the macula can lead to progressive visual disturbances up to the loss of the ability to read. In the long term, watching television, driving a car, doing handicrafts, recognizing faces and recognizing things you want to fixate on will also become more difficult. However, the external visual field is rarely affected. Therefore, there is no real risk of blindness. Diseases in this context include age-related macular degeneration, macular edema in diabetes mellitus and after vascular occlusion on the retina (thrombosis). They also include spontaneous formation of a hole in the middle of the retina (macular foramen) and spontaneous scarring (epiretinal gliosis or fibroplasia). Both usually as a result of a naturally occurring vitreous detachment. And sometimes drug toxic effects.
-
CAUSES
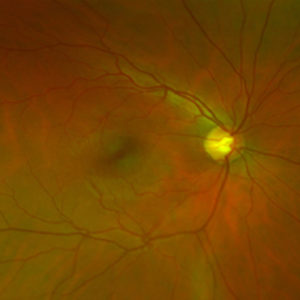 A healthy young retina with optic nerve head (papilla), retinal center (macula) and vessels (arteries and veins).
A healthy young retina with optic nerve head (papilla), retinal center (macula) and vessels (arteries and veins).The most common and best-known cause for changes in the macula is age. With increasing age, the risk for diseases of the macula increases significantly, especially for age-related macular degeneration, the most common treatable change of the retinal center. Other diseases of the macula, which also lead to a decrease in vision and distorted vision, are manifold. With age, scars on the retina or holes in the area of the visual center can develop. In addition, in the context of all vascular diseases, fluid from the vessels can enter the tissue and lead to swelling of the center of the retina (macular edema); for example after occlusion of the retinal vessels or in diabetes mellitus. Rarely rheumatoid or other inflammatory diseases, previous eye operations, medication or hereditary diseases are the cause of macular disease. An early diagnosis allows for, in many cases, and depending on the findings, a drug therapy or surgery.
Diseases that require an operation on the macula
If a mechanical impairment of the retinal center has led to a loss of visual acuity and a disturbance of binocular vision, it can spontaneously disappear again. If this is not the case or if there is already an advanced visual disturbance and damage, it can often only be stabilized by removing the vitreous body. The main problem here is:
- a scar tissue layer (membrane) on the center of the retina with distortion of the sensory cells of the retina
- a hole in the middle of the retina (macular hole)
- disturbing vitreous opacities, which impair the view
- an inflammation with swelling of the retinal center (macular edema)
-
SYMPTOMS
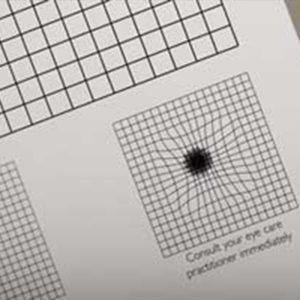 The Amsler test provides information about the patient's distorted vision.
The Amsler test provides information about the patient's distorted vision.A macular disease usually develops slowly and painlessly, but in some cases, it can be accompanied by a relatively rapid deterioration of vision.
Indications of a macular disease are:
- decreasing vision over days to weeks, usually in only one eye
- blurred, distorted vision (straight lines are waved)
- increased glare sensitivity and light perception
- normal field of view
- Spots (light or dark) in the center of vision
An early diagnosis is important, as the prognosis and treatability in many cases depend on it.
-
TREATMENT

The therapy options for macular diseases are manifold:
Depending on the cause of the retinal swelling and the risk of further deterioration, a primary attempt can be made to treat the disease with eye drops. In most cases, however, the chances of success are so poor. Alternatively, injecting a drug into the vitreous cavity creates a temporary sealing of the leaking vessels and thus a decongestant swelling is attempted. Or an inflammation is suppressed. A long-term solution may be laser therapy to obliterate the vessels and reduce the oxygen demand of the retina. However, this must not be carried out exactly in the center, otherwise a scar would cause a definitive loss of vision. For this reason, laser therapy is not an option in most cases, so that medication must be repeatedly injected into the vitreous body.
If there is scarring on the retina or a hole in the visual center, depending on the findings, surgical treatment with scar removal can often achieve stabilization of the retinal center. In the long term in many cases, even a certain improvement in vision.
If general basic diseases such as diabetes, high blood pressure, rheumatic and infectious diseases are responsible for macular edema, these must be treated, and in many cases a joint approach with the family doctor as coordinator is useful.
The success for the recovery of visual acuity often cannot be predicted. In most cases we can improve the macular disease, but often we cannot influence the underlying disease that caused it. Therefore, we can often stabilize the visual function, but cannot improve it in the long term to the extent that vision is as it was before the disease.
-
GENERAL PROBLEMS AND COMPLICATIONS
By way of introduction it should be said that all measures and interventions on the macula are very safe and complications are rare. Most problems and complications are treatable and have a good prognosis. Serious complications with possible permanent damage due to heavy bleeding or infection are fortunately extremely rare (for injections into the eye 1/3,000, for retinal surgery 1/1,000).
Nevertheless, therapy is only recommended if we estimate the risk of deterioration or loss of visual function without surgery to be significantly higher than with surgery.
Injections into the eye
A prolonged swelling of the retinal center leads to progressive visual disturbances up to the loss of reading ability. The aim of injection treatment into the vitreous body is to prevent further loss of vision.
By injecting a medication into the vitreous cavity, the swelling of the retinal center decreases, and the visual function can recover. At the same time, we can see how the retina responds to the treatment and benefits from it. The following medications are generally available to treat your underlying disease:
- Avastin ®
- Lucentis ®
- Eylea ®
- Beovu®
- Ozurdex
- Visudyne injection and laser treatment of the macula
- triamcinolone and dexamethasone
The first four drugs are intended to suppress the growth of unwanted blood vessels on the retina as a result of disturbed retinal metabolism. This is because fluid leaks from the newly formed vessels between the retinal sensory cells, (edema) due to a weaker vessel wall, resulting in vision deterioration. These drugs can also reduce the risk of bleeding at the center of the retina. Lucentis, Eylea, Beovu were primarily developed for ocular treatment, Avastin for tumor treatment. However, recent studies have shown that it also exerts a very beneficial effect on vascular neoplasms in the eye., The therapy has not yet received approval in Switzerland (“off-label” therapy). The fifth and sixth drugs; long-acting cortisone preparations in the eye, treat the inflammatory reaction of the tissue as cause and consequence of swelling of the retina. This can also reduce edema.
The procedure takes a few minutes and is performed on an outpatient basis. Before the procedure, the eye is numbed with drops, the skin is disinfected, and the eye is covered with sterile drapes. Then the medication is injected into the vitreous cavity with a very thin needle. Vision is not significantly affected by this, but points or shadows may be temporarily visible. A control is usually carried out after about 4 weeks, when we want to determine the success of the treatment and discuss whether it is advisable to repeat the treatment. If pain, an increasing visual disturbance or other unusual changes in the eye occur before this time, it is necessary to contact us immediately, as this is not normal.
Beovu®, which has been approved in Switzerland and the European Union since 2020, appears to be associated with a significantly higher risk of intraocular inflammation of blood vessels of the retina, than the preparations that have been available for longer. For this reason, if this agent is considered for you, you will be specifically advised of the possible symptoms by the treating ophthalmologist.
Problems with the treatment of macular edema
The success for the recovery of visual acuity cannot be predicted. In most cases, we can improve macular edema, but we cannot influence the underlying disease that caused it. Therefore, we can often stabilize the visual function, but not improve it to the point where vision is as good as it was before the disease occurred.
All drugs available to us, have a limited duration of action, usually between one and three months. Therefore, if the treatment is beneficial, injections are necessary again and again, in the long term, depending on the course of the disease. After about 3-4 injections of medication into the vitreous cavity, a temporary stabilization is often achieved. This allows for longer intervals between injections, or even a break of a few months, until the next injection are necessary.
Problems and complications
Injections into the eye often cause harmless conjunctival hemorrhages. In rare cases, bleeding into the vitreous cavity can occur and this can lead to temporary impairment of vision. The bleeding usually resolves within a few days up to 4 to 6 weeks. Some drugs themselves can occasionally cause blurred vision until it has dissolved.
Temporary increases in intraocular pressure may also occur. Therefore, controls of the eye pressure are necessary. In addition, the progression of a cataract (clouding of the lens) can be promoted. Sudden movements of the head during injection can, very rarely, damage the lens or the retina, so that cataracts, dislocation of the artificial lens or retinal detachment might occur.
The most serious but very rare complication is an infection of the inside of the eye (endophthalmitis), which can lead to loss of the eye (frequency about 1 per 10,000 injections). Only immediate surgery and antibiotics can help to achieve a good result. Typical signs of endophthalmitis are the appearance of severe pressure pain (not comparable to a foreign object in the eye), redness and deterioration of vision 2 to 6 days after the injection. If these symptoms occur, you should contact us immediately or consult your ophthalmologist.
Surgery of the retinal center
With the removal of the vitreous body we can remove all mechanical factors and optically disturbing opacities from the retina. However, an improvement in visual function can only be achieved if the structure of the retina has not yet been irreversibly damaged and can recover in the long term by the sensory cells regaining a straight line. This can take up to more than a year. Without treatment, an improvement in vision is often not achievable, in many cases there is even a further deterioration in visual function if the eye is not operated on.
The vitreous body, which has lost its supporting function in the course of life but is partly responsible for the existing visual disturbances, is removed from the eye and replaced. The replacement is usually an air or gas filling that is absorbed by the body within fourteen days after the operation and replaced by a newly formed aqueous vitreous fluid, which then no longer causes problems.
Operations at the center of the retina (vitrectomy) must be performed safely and reliably under local anesthetic. When the anesthesia wears off, depending on the duration of the operation and the measures carried out, pain often occurs that requires treatment. In addition, the eye pressure is low, so that the risk of secondary bleeding is increased during exertion. In the first two days the eye is sensitive and needs rest, physical exertion should be avoided. For this reason, we prefer in-patient treatment. With an air or gas filling you are not allowed to stay at altitudes above 700 m above sea level for about 8 days, which you should consider when planning your journey home. Within the first fourteen days after the operation, visual acuity is reduced to the perception of light and movement, and then usually recovers quickly to the visual acuity before the operation.
The best possible visual acuity may not be achieved until one year after the operation. Although we hope for an improvement in visual acuity, the operation is mainly performed to stabilize the retinal situation and to prevent further deterioration of vision.
If cataracts have not been operated on before the retinal surgery, it is to be expected that the removal of the vitreous body within 6 months after the operation will lead to the development or progression of lens opacity (cataract). If this becomes optically disturbing, it can then be operated on.
In the first days after the operation, fluctuations in the eye pressure may occur, which must be treated. If there is postoperative bleeding, this means a delayed recovery of visual acuity.
In almost all cases, the removal of the vitreous body is possible without major or unforeseeable problems and without endangering the stability of the retina. Nevertheless, tears in the retina are occasionally discovered at the end of the operation, which are treated with cold or laser, as they could otherwise cause a retinal detachment later. But also, secondary, in about 3-5% of cases, typically within 4 weeks postoperatively, a tear of the retina and a retinal detachment occurs, which has to be operated immediately. If the retina is not stable enough, in rare cases the replacement of the vitreous body with silicone oil is necessary to ensure retinal stability after surgery. In this case, further surgery to remove the silicone oil is necessary at a later date.
Severe bleeding, infection, deterioration of vision or even further loss of vision or of the eye are extremely rare (less than 1:1000), but possible in principle. If one of the above-mentioned complications occurs, another operation is usually necessary in order to achieve the best possible result.
-
EXAMINATION
The examination and treatment of a macular disease is carried out by us on medical referral, preferably by your ophthalmologist, who will also take over the follow-up care together with us. After we have received a letter of referral, we arrange for an outpatient examination during our office hours.
-
A. ASSESSMENT OF VISUAL FUNCTION AND PREDICTABILITY OF TREATMENT SUCCESS
 The first thing we do is examine the refractive power and eye pressure with the autorefractometer.
The first thing we do is examine the refractive power and eye pressure with the autorefractometer.Background
The macula forms the center of vision. It is only developed in primates and humans, which is why only these reach a sufficiently high image resolution to be able to read. The extremely high demands on the metabolism of the photoreceptors for the high performance are largely understood today. However, the processes that cause deterioration in old age or in degenerative diseases such as retinitis pigmentosa, epiretinal fibroplasia, diabetic maculopathy, etc. are only very vaguely understood in principle. First therapeutic approaches are now possible with intravitreal injections to seal leaking vessels (anti-VEGF therapy, for example Lucentis or Avastin), but there is no prophylaxis to prevent these diseases.
However, the biggest problem in the treatment of diseases of the retinal center is the assessment of central visual function and the possible functional gain after an intervention. The commonly used visual acuity measurement allows very accurate and reproducible measurement of visual acuity at one point (reading a letter), which is of little importance for everyday use. Accordingly, patients are often not satisfied with their visual function despite a very good measured visual acuity, or they need relatively large magnifying glasses in order to be able to read despite an astonishingly good visual acuity. They often recognize a single letter in focus but cannot read an entire word because they have large gaps in the center and very poor contrast vision. You can imagine this like a puzzle in which 50% of the pieces are missing. Even if the brain can complete the picture, the quality of the information and the speed of image acquisition are thus very reduced.
Therefore, for the evaluation of macular function, additional tests such as reading speed and the measurement of loss spots and areas in the central visual field would probably be much better suited to describe performance. However, this has not yet been systematically investigated because of the great effort involved. It is possible, however, that a better assessment of visual function may also lead to a considerably better predictability of the success of treatment, for example after surgical interventions. Therefore, we have been working for some time on a more detailed analysis of macular function and its predictive significance for the treatment of diseases of the retinal center.
-
B. ASSESSMENT OF VISUAL FUNCTION AND PREDICTABILITY OF TREATMENT SUCCESS
 OCT (optical coherence tomography): examination using laser scanning technology (Heidelberg Spectralis HRA).
OCT (optical coherence tomography): examination using laser scanning technology (Heidelberg Spectralis HRA).Current situation and limits of treatment
The possibility of treating macular diseases has increased massively in the last years due to technical improvements and new drug developments. Up to now, due to a lack of treatment options, there has been a lack of commitment to quantify the visual disorders complained of by patients. With the new possibilities of treatment, the problem has now arisen to offer each patient a treatment suitable for him or her and to predict the functional benefit of the therapy. For this reason, patients with macular diseases are usually referred to specialized centers such as the Bern Eye Clinic at the Lindenhof Hospital. Here we have the possibility to perform examinations of the morphology of the retinal center with a resolution of 3-5μm using high-resolution laser scanning technology without any stress for the patients and can thus often explain the complaints morphologically. At this point patients can often be offered solutions appropriate to their situation. As a rule, there is also a very good morphological recovery of the retinal center during treatment. Accordingly, the treatment is very satisfactory in most cases. In up to one third of the cases, despite a very pleasing morphological situation, the functional gain remains below the patient‘s expectations. This may be due to the fact that the visual function is not sufficiently described by the measurement of visual acuity and we achieve an improvement of visual acuity but not of the visual function, especially of reading visual acuity. On the other hand, we have so far not had the opportunity for preoperative assessment of the possible functional gain after an intervention.
Therefore, we have tried to adjust the apparatus equipment to describe the functional and morphological situation of the retinal center as well as possible. In a second step, we have tried to evaluate whether it is possible to predict the postoperative success for vision based on certain preoperative findings.
-
C. ASSESSMENT OF VISUAL FUNCTION AND PREDICTABILITY OF TREATMENT SUCCESS
 Microperimetry analysis using the Nidek MP1.
Microperimetry analysis using the Nidek MP1.Apparatus methods
The development of apparatuses has – following the development of therapy and the needs of medicine – brought considerable improvements in recent years. Among the possibilities of morphological examination and documentation, high-resolution OCT analysis is the most important. It is only in recent years that OCT technology (Spectral Domain OCT) has allowed a sufficiently differentiated assessment of the anatomical situation with regard to the resolution of anatomical structures (<5μm) that a correlation of morphological and functional parameters becomes meaningful and helpful. The OCT examination is now considered to be the most important examination for the assessment of the retinal center and for the evaluation of the success of therapy in macular diseases. However, the method is mainly used to detect the presence of damage or swelling in the center of the retina (macular edema) and its therapeutic influence. Investigations of the foveal contour (site of sharpest vision) and photoreceptor density and their correlation with functional parameters or the estimation of a possible functional gain, have so far only been reported in single case observations. Thanks to the use of digital methods, the quality of fundus photography and angiography has already reached a sufficiently high level of informative value. However, due to the high sensitivity of the photodetectors, the light exposure for the patients has become significantly lower, so that these examinations can be carried out without major impairment for the patient.
Recently, a new examination method was added to our diagnostic arsenal: OCT angiography (OCT-A). OCT-A is a further development of OCT technology, which enables rapid (<1 minute), and non-invasive, three-dimensional imaging of the vascular structures of the retina and choroid.
The functional examination methods for determining visual acuity, reading acuity and reading speed as well as central visual field, are now computer-controlled and largely standardized. For some years now, microperimetry has also been available, which allows a quite reproducible assessment of the sensitivity of the central retina and fixation behavior. This method generates new measurement results, which so far can only be assessed in the course of the disease and have not yet been systematically compared with the existing established tests. However, the significance of these results probably exceeds the established methods (visual acuity, magnification requirement, reading acuity, visual field examination) by far. So far, only one device for microperimetry analysis is available and has been on the market for a few years. This is currently being evaluated at numerous European centers, including ours. Comparative tests with other functional tests have not been carried out to date due to the high personnel costs involved. This is especially true for fixation behavior (how well a patient can fixate a point) and recovery from light stress in patients with macular diseases.
In summary, the function and the possible success of a treatment of macular diseases can be predicted quite well. However, most tests are based on the subjective statements of the patients and require a great ability to concentrate. Especially if visual acuity is significantly reduced, which limits their reproducibility and significance.

